Project Summary Page 1 Page 2
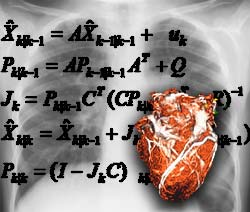 Penetrating wounds to the thorax and its organs are a major contributor to injury and mortality in the combat setting. The purpose of this proposed project is to transform the way we view, study, and interact with information about the human body and its complex and interrelated systems, and in doing so create an applied system that will revolutionize medical care to the soldier. The ultimate goal is the construction of a complete, functioning, accessible simulation of the human thorax-from the physiology of individual cells to the operation of entire organ-tissue systems. This virtual representation of the human thorax will provide capabilities to diagnose battlefield injuries, specifically ballistic wounds to the heart. The proposed field deployable system will be aware of empirical normal anatomical variability among soldiers' hearts, physiological parameters, and other critical thorax anatomical structures/variabilities. It will also contain the range of effects that penetrating thorax wounds have been observed to engender in previously healthy hearts. In the resulting field system, general prior knowledge of this sort will be unfolded into steadily more precise estimation of the particular parameters of damage, and will aid in the prediction of outcomes and suggest treatment measures for particular ballistic trauma cases.
Penetrating wounds to the thorax and its organs are a major contributor to injury and mortality in the combat setting. The purpose of this proposed project is to transform the way we view, study, and interact with information about the human body and its complex and interrelated systems, and in doing so create an applied system that will revolutionize medical care to the soldier. The ultimate goal is the construction of a complete, functioning, accessible simulation of the human thorax-from the physiology of individual cells to the operation of entire organ-tissue systems. This virtual representation of the human thorax will provide capabilities to diagnose battlefield injuries, specifically ballistic wounds to the heart. The proposed field deployable system will be aware of empirical normal anatomical variability among soldiers' hearts, physiological parameters, and other critical thorax anatomical structures/variabilities. It will also contain the range of effects that penetrating thorax wounds have been observed to engender in previously healthy hearts. In the resulting field system, general prior knowledge of this sort will be unfolded into steadily more precise estimation of the particular parameters of damage, and will aid in the prediction of outcomes and suggest treatment measures for particular ballistic trauma cases.
The ballistics/clinical team will provide key guidance for developing a credible, predictive heart model with relevance to the medical practitioner in the far forward combat setting. To this end, we have involved the new U.S. Army Ballistics laboratory at Ft. Sam Houston, and world experts in trauma and ballistic modeling from Porton Down in the United Kingdom; USUHS, and elsewhere. Data will be made available from public and private databases of combat injuries from Europe, Israel and the U.S.
The Organ-Tissue system will represent a complex human visualization/simulation. The anatomical simulator can be queried for structural information, and will also display certain anatomical and physiological features important for visualization of penetrating wounds, including projectile trajectories, hemodynamics, and organ reactivity at the gross level (e.g. lung collapse) and at the cellular level (e.g., cell death and ventricular pathology). Penetrating wounds will thus be modeled both at the tissue level (when tissue is removed) and at properties level (when tissue is rendered inert or passive).
To build a virtual human torso, the Foundational Model (Cornelius Rosse and collaborators) will be used as the ontology providing a framework for the structural elements of the heart and thorax. The virtual torso will be able to predict damage to tissues from a ballistics wound, and predict changes in specific measurable physical parameters such as hemodynamics, blood pressure, pulse, EKG, etc. Several heart models will be assessed, including immersed boundary variants and fluid-solid coupled models, and a decision will be made to either build from scratch, or potentially allow the user to query different available models for characteristics such as electrical integrity and hemodynamic changes caused by the wounding, including blood loss. The visualization tool will allow for easy access to the complex data predicted by the model, including visualization of the biomechanical damage from all perspectives relevant to a forward surgical team, providing changes in physiological signs for differential diagnosis, and prediction of dangerous conditions that would require immediate care, all integrated in a compelling interface display for complex statistical, anatomical and physiologic information.
Currently the Foundational Model does not include actual Cartesian geometry, nor does it incorporate knowledge of anatomical variability. In addition, it does not include adequate linkages to physiological representations. The Task #1 team (Stanford Lead) will develop prototypes for the formal extension of the FM in these new directions.
The virtual torso model will include different levels of spatial hierarchy, comprising skin, chest wall with ribcage and muscle layers, heart and great vessels, trachea, bronchi, lungs and aorta. The Virtual Torso simulation will consist of a three dimensional (3D) polygonal computer graphics model of the thorax, with integrated physiology, exhibiting appropriate respiratory and cardiac activity. Cardiovascular and respiratory rates will be interactive and responsive to penetrating wounds. To achieve anatomical validation at the organ level, two sources of data will be used – segmented diagnostic image-based models derived from CT and MRI scans with photorealistic texture maps and segmented Visible Human datasets from the National Library of Medicine. Furthermore, multiple scales will be modeled in the heart, ranging from the cellular level (e.g., cardiac myocyte) to the organ level. This model will be capable of free warping (in the course of visualization) into any normal torso geometry, ultimately for the purpose of video fusion with the image of the wounded soldier per se. The geometry of the model will be adjustable at least to the extent of rendering collinear the effects of a projectile on entrance site, cardiac tissue, and exit site, so that the "moment of impact" can itself be visualized, together with the involvement of other organs and tissues near the projectile track. For instance, it is quite important to know if the myocardium is in a state of contraction or instead relaxation when the projectile impacts; we will be able to estimate that condition (with some error, of course). Page 2, Project Summary Cont.
